Background
Fanconi anemia (FA) is an inherited bone marrow failure syndrome which develops on the basis of defective cellular responses to DNA damage. Aldehyde degradation deficiency (ADD) syndrome has been recently found as a disease caused by the defect of degradation of endogenous formaldehyde, which shares similar clinical features with FA. Although genomic abnormalities in these diseases have been associated with the high propensity of myeloid malignancies such as myelodysplastic syndrome (MDS) and acute myeloid leukemia (AML), the mechanism of the early development of MDS/AML remains unclear. Therefore, in this study, we aimed to understand the mechanism of the development of hematological malignancies by analyzing the genomic abnormalities seen in these diseases.
Method
We performed whole-exome sequencing (WES) and whole-genome sequencing (WGS) for 2 AML and 6 MDS developed in Japanese patients with FA (n = 6) and ADD syndrome (n = 2). Skin or bone marrow fibroblasts derived from the same patients were also studied as germline controls. We investigated somatic mutations, structural variants (SVs), and copy number alterations (CNAs) by WES and WGS. Mutational signature was analyzed to understand the mutational processes in these diseases.
Result
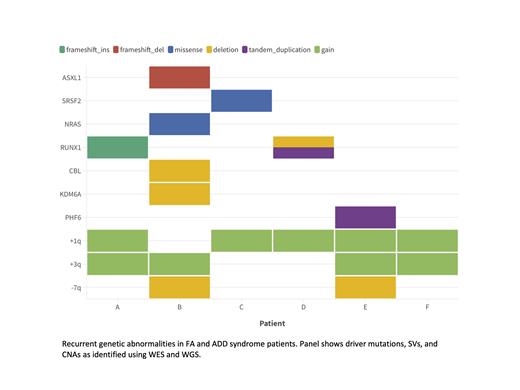
The number of somatic mutations and CNAs in AML identified by WES were 24 and 5 per patient on average, respectively, which were higher than those in MDS (6.8 mutations and 1.8 CNAs per patient) (P=0.07 and 0.06, respectively). However, no significant difference was observed for the number of SVs identified by WGS between MDS (35 counts per patient) and AML (52 counts per patient). Somatic mutations affected known driver genes in myeloid malignancies, such as RUNX1 (n = 1), ASXL1 (n = 1), SRSF2 (n = 1) and NRAS (n = 1) (Figure1). SVs also involved known driver genes in myeloid malignancies, such as CBL (n = 1), KDM6A (n = 1), PHF6 (n = 1), and RUNX1 (n = 1). In total, RUNX1 was most frequently altered (2/6, 33%). CNAs were more frequently accumulated in recurrent regions, including +1q (n = 5), +3q (n = 4), and -7q (n = 2) (Figure1). As previously reported, MDM4 and EVI1 were contained in +1q and +3q, respectively. Higher cancer cell fraction implied that most of these copy number changes were clonal, which suggested the early acquisition of copy number changes and their driver role in leukemic transformation. For mutational signatures, three known signatures were identified, which included clock-like SBS1 and SBS5 caused by endogenous mutational processes, and SBS3 related to defective homologous recombination. In addition, a novel mutational signature (Sig-A) was also detected. SBS3 and Sig-A were mainly detected in patients with FA and ADD syndrome, respectively, indicating that the different mutational processes are operating in the two diseases.
Conclusion
WES and WGS revealed the genetic landscape of FA and ADD syndrome mutation accumulation. Myeloid neoplasms related with FA and ADD syndrome were characterized by a unique pattern of driver mutations and CNAs, such as RUNX1 mutations/SVs, +1q and +3q. Although the two diseases share some clinical features, our study has revealed the different mutational processes in these diseases. Further investigation is warranted to reveal the underling mechanisms of mutation accumulation and the role of driver mutations in these diseases.
Disclosures
No relevant conflicts of interest to declare.